General medicine case-6
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
Date of admission: 15/10/21
A 50 year old female came to the OPD with chief complaints of lower backache, decreased urine output, shortness of breath and fever since 4 days.
History of present illness:
The patient was apparently asymptomatic 4 days back when she noticed a pain in the lower back and decreased urine output and shortness of breath.
History of past illness:
The patient is a known case of hypertension since 7 years.
Not a known case of diabetes,asthma, epilepsy, tuberculosis.
Personal history:
The patient has no loss of appetite.
She has mixed diet.
Sleep is inadequate.
The patient has no habits of tobacco chewing or alcohol consumption.
Family history:
There are no similar complaints in the family.
Treatment history:
The patient is not allergic to any known drugs.
General examination:
Patient is conscious, coherent, cooperative at the time of joining.
No pallor
No icterus
No cyanosis
No clubbing of fingers and toes
No lymphadenopathy
Pedal edema is present.
Vitals : temperature - 98.6⁰F
Pulse rate - 84 bpm
Respiratory rate - 22 cycles per minute
BP - 140/90 mm Hg
Systemic examination:
CVS:
Inspection - chest wall is bilaterally symmetrical
- No precordial bulge
- No visible pulsations, engorged veins, scars, sinuses
Palpation - JVP is normal
Auscultation - S1 and S2 heard
RESPIRATORY SYSTEM:
- Position of trachea is central
- Bilateral air entry is normal
- Normal vesicular breath sounds heard
- No added sounds
PER ABDOMEN
- abdomen is tender
- bowel sounds heard
- no palpable mass or free fluid
CNS:
- Patient is conscious
- Speech is present
- Reflexes are normal.
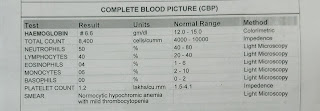
Investigations:
Diagnosis:
Chronic kidney disease.
Treatment:
1) FLUID RESTRICTION < 1.5 L/day
2) SALT RESTRICTION < 2 gm / day
3) TAB LASIX 40 mg PO BD
4) TAB NICARDIA 20 mg PO TID
5) TAB OROFER XT PO BD
6) TAB NODOSIS 500 mg PO BD
7) TAB BIO O3 0.25 mg OD
8) TAB DOLO 600 mg PO TID
9) NEB. DUOLIN 6th hourly
BUDECORT 8th hourly
10) INJ ERYTHROPOIETIN 4000 units S/C weekly once
11) TAB ARKAMKNE 0.1 mg PO TID.













Comments
Post a Comment