General medicine final exam short case
This is online E log book to discuss our patients de- identified health data shared after taking his or her guardian's signed informed consent hear we discuss our individual patients problems through a series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.This E log book also reflex my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
Date of admission: 07/02/2022
CHIEF COMPLAINTS:
A 27 year old male patient electrician by occupation presented to the OPD with chief complaints of pain in stomach and vomitings since 3 months.
HISTORY OF PRESENT ILLNESS:
The patient was apparently asymptomatic 3 months back, when he had a trauma where his relatives had beaten him up with a stick at the left hypochondrium region due to which he developed abdominal pain associated with vomiting. The pain subsided on taking medications.
After a few days he again developed pain abdomen at the left hypochondrium region and pain radiating to back for which he went to hospital where he underwent treatment but the symptoms didn't subside.
So he went to other hospital where he took treatment..he was tested covid positive in the middle of the treatment ,so he went to home isolation .
After few days he underwent the treatment after testing covid negative, the symptoms were subsided then.
Then after he again developed the pain since 3 days before he was presented to our hospital with c/o of abdominal pain(hypochondrium region) which is radiating to his back.
The pain is aggrevated while walking, sleeping after a prolonged duration of sitting and relieved when he bends forward.
Patient complains of pain after eating.
PAST HISTORY :-
No history of diabetes/hypertension/asthma/epilepsy
No previous surgical history
PERSONAL HISTORY:
Diet : mixed
Appetite : decreased since 10 days
Sleep : inadequate
Bowel & bladder : irregular since 3 days
Addictions :- history of alcohol intake since 4 years consumes 360ml per day, he stopped consuming since 4months.
Regular usage of khaini since 4 years.
FAMILY HISTORY :
No relevant family history
GENERAL EXAMINATION :
Patient is conscious, coherent, cooperative and thin built.
No pallor , Icterus,clubbing, cyanosis ,edema.
VITALS :
Temp- Afebrile
Bp-100/80 mm hg
Pr- 84bpm
Rr-16cpm
Spo2- 99% on RA
Grbs : 102
SYSTEMIC EXAMINATION :
Respiratory system- bilateral air entry present
No dyspnea
No wheeze
Position of trachea- central
ABDOMEN-
Tenderness - present at hypochondrium region
Shape of abdomen- scaphoid
Spleen not palpable
Bowel sounds are present
CNS:
Level of consciousness- conscious
Speech - normal
No neck stiffness
CVS:
S1 and S2 are heard.
INVESTIGATIONS:
Hemogram:
Hb=10.5 gm/dl
PCV=#32.5
Liver function test:
Total bilirubin- 0.48mg/dl
Direct bilirubin- 0.17mg/dl
SGOT=13 IU/L
SGPT=14 IU/L
Alkaline phosphatase= # 291IU/L
Total proteins- #5.9gm/dl
Albumin # 2.9gm/dl
A/G ratio =0.98
Serum amylase=292
CRP POSTIVE 2.4mg/dl
PROVISIONAL DIAGNOSIS:
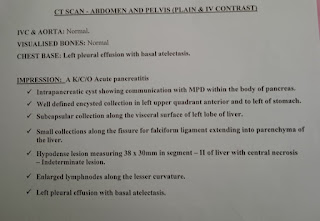
Chronic pancreatitis with pseudocyst
TREATMENT:
1. IVF NS/RL - 75ml/hr
2. Inj Tramadol 100ml IV/TID
3. Inj Pantop 40mg IV/OD
4. Inj.zofer 4mg IV/SOS











Comments
Post a Comment