General medicine case- 4
This is an online e-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
Date of admission: 23/09/2021
A 85 year-old man, who is a farm worker by occupation, presented to the hospital with complains of
- Weakness of left upperlimb and lowerlimb since 20 days
-Deviation of mouth towards left side since 20 days
- Difficulty in swallowing since 20 days.
History of present illness:
The patient was apparently asymptomatic 20 days back then had sudden weakness in left upperlimb and lower limb one morning.
He couldn't walk and also noticed difficulty in swallowing.
He was taken to the local hospital and was later referred to Kamineni for further treatment.
Past history:
The patient is a known case of hypertension since 3 years.
Not a known case of Diabetes mellitus, Asthma, Tuberculosis, Epilepsy.
Personal history:
The patient has a mixed diet.
Has a loss of appetite since 20 days.
Bowel and bladder movements are normal.
The patient is a chronic smoker(4-5 chutta/day)and alcoholic since 20 years.
Has stopped drinking and smoking 2 months ago.
Treatment history:
The patient is not allergic to any known drugs.
General examination:
The patient is conscious, coherent and cooperative
Pallor- Yes
Cyanosis- No
Lymphadenopathy- No
Clubbing of fingers- No
Pedal edema- No
Vitals:
Temperature- Afebrile
Pulse rate- 100 bpm
Blood pressure- 140/90 mmhg
Respiratory rate- 22 cycles per min
Systemic examination:
CVS- S1 and S2 heard
Respiratory system:
NVBS present
CNS
Conscious
Speech - normal
No signs of meningeal irritation
Tone- Increased in left side.
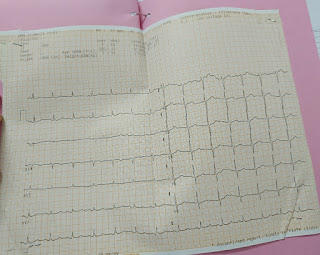
Investigations:
Treatment:
RT FEEDS 100 ML MILK - 2ND HOURLY , 100ML HOURLY
2) INJ PAN 40 MG /IV/OD
3) INJ OPTINEURON 1 AMP IN 100 ML NS /IV/OVER 30 MIN
4)TAB ASPIRIN 100 MG RT/OD
5)TAB CLOPIDOGREL 75 MG RT /OD/H/S
6) TAB ATORVASTATIN 40 MG /RT/OD/HS














Comments
Post a Comment