General medicine case-7
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment"
Date of admission: 02/11/2021
A 40 year old female who is a farm worker by occupation presented to the OPD with chief complaints of fever, dry cough and breathlessness since 2 days.
History of present illness:
Patient was apparently asymptomatic 2 days back then developed high grade fever with chills which is intermittent, relieving on medication.
The patient also developed headache and vomitings(2-3 episodes/day).
Past history:
Not a known case of Hypertension, Diabetes mellitus, Asthma, Tuberculosis, Epilepsy.
Personal history:
The patient has a mixed diet.
Appetite is normal.
Bowel and bladder movements are normal.
Has no habits of smoking and alcohol consumption.
Treatment history:
The patient is not allergic to any known drugs.
General examination:
The patient is conscious, coherent and cooperative
Pallor- Yes
Cyanosis- No
Lymphadenopathy- No
Clubbing of fingers- No
Pedal edema- No
Vitals:
Temperature- 98⁰F
Pulse rate- 108 bpm
Blood pressure- 90/60 mmhg
Respiratory rate- 22 cycles per min
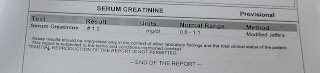
Investigations:
Treatment:
1) IVF 20 NS
20 RL
10 DNS
@100 ml/hr
2) INJ PANTOP 40 mg IV OD
3) INJ OPTINEURON 1 amp in 100 ml NS IV OD
4) PLENTY OF ORAL FLUIDS
5) TAB DOLO 650 mg PO SOS
6) INJ NEOMOL 1 gm IV SOS ( if temp>101⁰F)
7)W/F BLEEDING MANIFESTATIONS; POSTURAL DROP IN BP.











Comments
Post a Comment