General medicine final exam long case
THIS IS AN ONLINE E LOG BOOK TO DISCUSS OUR PATIENT'S DE - IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS / HER /GUARDIAN'S SIGNED INFORMED CONSENT .HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH SERIES OF INPUTS FROM AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS WITH AN AIM TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE BASED INPUT.
Date of admission: 08/02/2022
Chief complaint:
A 50 year male farmer by occupation presented to casualty in stuporous state with complaints of
-pain abdomen since15 days
-Loss of appetite since 10 days
-H/o fever since 3days.
-h/o vomitings since 3 days
-h/o constipation since 3 days
-h/o altered sensorium since 3 days
-h/o yellowish discoloration of urine since 2 days
History of present illness:
Patient was apparently asymptomatic 15 days back,then he developed pain abdomen in epigastric region associated with 3 episodes of vomitings-food particles as content.
Constipation present since 3 days,passing flatus.
Past history:
Not a known case of DM, HTN,CVA,CAD,COVID-19.
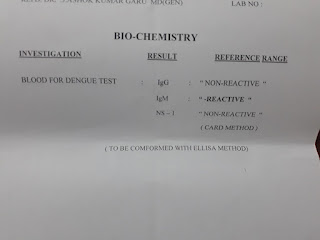
Diagnosed as DENGUE IgM POSITIVE ON 2/2/22- and treatment is taken.
Personal history:
Diet- mixed
Appetite- loss of appetite since 10 days
Bowel- constipation since 3 days
Bladder movements- regular
Addictions: H/O smoking since 35 years (2-3 beedis per day)
Alcohol: Regular intake of 90 ml daily since 35 years.
Family history:
No similar complaints in the family.
Treatment history:
The patient is not allergic to any known drugs.
General examination:
The patient is drowsy, non responsive and non cooperative at the time of examination.
- No pallor
- No cyanosis
- No clubbing of fingers and toes
- No lymphadenopathy
- No pedal edema
- Icterus is present
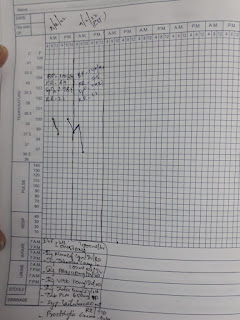
Vitals:
Temperature: 102⁰F
Pulse rate: 98 bpm
BP: 130/80 mm Hg
Respiratory rate: 22 cpm
Systemic examination:
CVS:
Inspection - chest wall is bilaterally symmetrical
No precordial bulge
- No visible pulsations, engorged veins, scars, sinuses
Palpation - JVP is normal
Auscultation - S1 and S2 heard
RESPIRATORY SYSTEM
- Position of trachea is central
- Bilateral air entry is normal
- Normal vesicular breath sounds heard
- No added sounds
PER ABDOMEN :
Shape of the abdomen: scaphoid
- abdomen is not tender
- bowel and bladder sounds heard
- no palpable mass or free fluid
CNS:
Patient is DROWSY,NO RESPONSE,
non cooperative
Neck STIFFNESS+,kernig sign+.
Investigations:
LFT:
TB-8.95
DB-3.85
AST-64
ALT-190
ALP-319
TP-4.7
ALB-2.77
A/G-1.44
PT-20
INR-1.4
APTT-38
RFT:
UREA-49
CREAT-0.9
URIC ACID-2.8
CA++-7.7
K+-2.9
CL-96
Na-140
Opthamology referral was done.
Findings in left eye:
Lids-discharge at canthus
Conjunctiva- early inflammed nasal pterygium
Mild congestion +
Cornea-clear
Sclera-yellowish discoloration +
PROVISIONAL DIAGNOSIS: DENGUE ENCEPHALITIS ?
TREATMENT:
1.IVF-NS,RL@100ML /HR
2.INJ.MONOCEF 1 GM /IV/BD
3.INJ.ZOFER 4MG/IV/TID
4.INJ.THIAMINE 2 AMP IN 100ML NS/IV/STAT
5.INJ.NEOMOL 1 GM/IV/STAT
6.TAB.PCM 650MG/PO/TID
7.SYP.LACTULOSE 20ML/PO/TID
8.PROCTOLYTIC ENEMA-P/R-TWICE DAILY
9.INJ.DOXYCYCLINE 100MG/IV/BD
10.INJ.VIT K 10MG IV_OD
11.INJ.PAN 40 MG /IV/BD
LUMBAR PUNCTURE DONE











Comments
Post a Comment